Background
The treatment landscape for acute myeloid leukemia (AML) is rapidly evolving, and with many of the more recently FDA approved treatments being targeted therapies, timely and actionable molecular and cytogenetic testing is critical to the management of AML patients. However, many challenges and barriers to optimal testing workflows impede clinicians' ability to integrate genetic testing in treatment decision-making. To improve quality care related to genetic testing in AML, we conducted a quality improvement (QI) study focused on evidence-based integration of genetic testing into routine practice for AML patients in community oncology clinics.
Methods
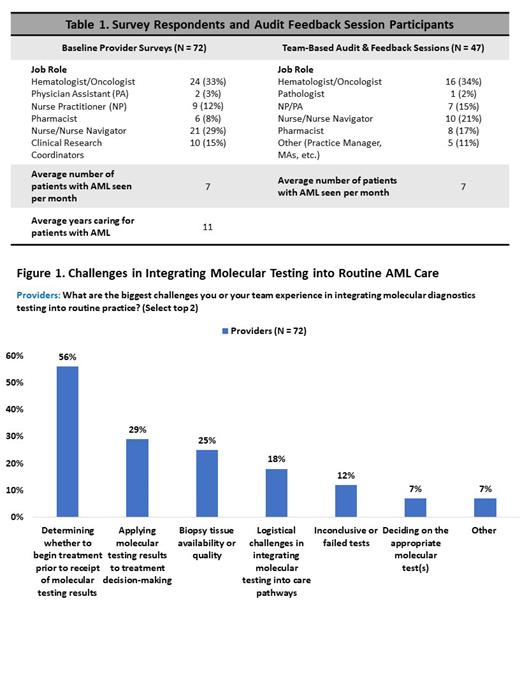
This QI initiative is comprised of baseline (N = 72) and follow-up provider surveys, and pre- and post-surveys of providers participating in small-group, team-based audit-feedback (AF) sessions across 5 community clinics. Survey questions were designed to assess knowledge, confidence, and experiences with genetic testing in AML. Care teams from each clinic, along with an expert AML oncologist and a hematopathologist, participated in AF sessions to (a) assess system-specific practice gaps identified via the provider surveys, (b) prioritize areas for improvement, and (c) develop action plans for addressing root causes.
Results
Provider Surveys: Providers top reported challenges encountered with integrating genetic testing into routine practice include determining whether to begin treatment prior to receipt of genetic testing result (56%)and applying genetic testing results to treatment decision-making (29%). For patients with AML, 70% of providers stated they were likely to start treatment prior to receiving testing results. When asked to report routine molecular testing practice patterns, 72% of providers reported testing for FLT3 mutations, 62% for IDH1/2 mutations, 65% for TP53 mutations, and 63% for NPM1 mutations; with further suboptimal reported practices in the use of NGS panels (58%; average turnaround time 15 days) and PCR (52%; average turnaround time 8 days). Overall, providers reported a 56% satisfaction rate with the processes implemented in the clinic related to sample preparation, timely review, and turnaround time of molecular diagnostics testing reports.
AF Sessions: Providers participating in the AF sessions also reported determining whether to begin treatment prior to receipt of molecular testing results, long turnaround times and deciding on the appropriate molecular tests as top barriers to integrating testing in routine AML care. Clinicians reported improvements in high/very high confidence in their ability to select appropriate genetic tests to order for patients with AML (35% to 50%) and select targeted therapies based on genetic test results for AML patients (34% to 59%). Care teams set goals to improve turnaround times and testing workflows with pathology partners, as well as to maximize opportunities for patients to receive AML therapies for their specific mutation profile. Action plans to achieve these goals include improve team skills in choosing guideline-based genetic testing methods and targeted therapies and collaborate among clinical teams to improve ordering workflow and diagnostic sample preparation for genetic testing.
Follow-Up Surveys: In 90-day follow up surveys, 100% of clinic champions reported upshifts in patients with targetable driver mutations receiving guideline-recommended treatment based on genetic testing results, and 4/5 clinics reported improved selection of guideline-recommended genetic testing prior to treatment initiation for AML patients.
Conclusions
Through this QI initiative, clinical teams identified barriers to integrating genetic testing into routine AML care, creating and implementing action plans to optimize genetic testing workflows and guideline-recommended targeted therapy selection. While meaningful confidence and action plan gains were demonstrated, these data underscore clinical practice gaps to address in future initiatives to support the integration of evidence-based genetic testing into AML care, including integrated education sessions with clinicians and pathologists.
Study Sponsor Statement
The study reported in this abstract was funded by independent educational grants from AbbVie, Inc. and Astellas Pharma Global Development, Inc., who had no role in the study design, execution, analysis, or reporting.
Disclosures
Lai:Rigel: Consultancy; BMS: Consultancy; Jazz: Consultancy, Research Funding, Speakers Bureau; Novartis: Consultancy; Pfizer: Consultancy; Genentech: Consultancy; Taiho: Consultancy; Daiichi: Consultancy; Astellas: Consultancy, Speakers Bureau; AbbVie: Consultancy.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal